Release date:2023-10-31
Int. J. Med. Sci
[IF: 3.642]
Elevated Serum Aspergillus Fumigatus-Specific Immunoglobulin G in Type 2 Chronic RhinosinusitisDOI: 10.7150/ijms.83327
Abstract:
Background:Aspergillus fumigatus-specific immunoglobulin G (Af-sIgG) has been applied to diagnose allergic bronchopulmonary aspergillosis, a hypersensitivity reaction to the colonization of the fungus in the lower airways. In the upper airways, it has been reported to be involved in allergic fungal rhinosinusitis and local fungal rhinosinusitis. However, in primary chronic rhinosinusitis (CRS), a more common upper airway disease, the role of Af-sIgG remains unclear.
Objective: The aim of our study was to investigate the role of serum Af-sIgG levels in primary CRS patients.
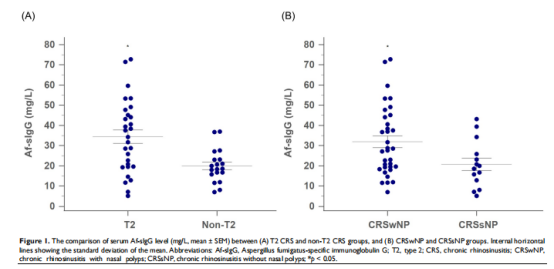
Methods:We prospectively recruited patients diagnosed with bilateral primary CRS and patients with nasal septal deviation as the non-CRS group. Patients in the primary CRS group were further classified into two endotypes, including type 2 (T2) and non-T2 groups. Serum samples collected were sent for Af-sIgG analysis. Potential factors and surgical outcomes were analyzed.
Results:: Forty-eight patients with a diagnosis of primary CRS (including 28 with T2 and 20 with non-T2 CRS) and 22 patients in the non-CRS group were recruited. The T2 CRS group had significantly higher serum Af-sIgG levels than the non-T2 CRS group (odds ratio 10.2 with Af-sIgG more than 27.6 mg/L;p < 0.001). Further multivariate logistic regression showed that the serum Af-sIgG level was the independent factor for early disease recurrence within one year in primary CRS patients. The optimal cutoff value of the serum Af-sIgG level to predict postoperative recurrence was 27.1 mg/L (odds ratio 15.1, p = 0.013).
Conclusions:We suggest that the serum Af-sIgG level is a practical marker to detect T2 inflammation and the surgical outcome of primary CRS. By applying this feasible test, we may be able to achieve optimal treatment for every individual with primary CRS. This study may provide physicians with a reference for future clinical applications in dealing with primary CRS.
First Author:
Yun-Chen Chang
Corresponding author:
Chia-Hsiang Fu
Correspondence:
Division of Rhinology, Department of Otolaryngology-Head and Neck Surgery, Linkou Chang Gung Memorial Hospital and Chang Gung University, No. 5 Fu-Shin Street, Guishan District, Taoyuan City, 333, Taiwan.
E-mail: fufamily@adm.cgmh.org.tw.
 杭州浙大迪迅生物基因工程有限公司
杭州浙大迪迅生物基因工程有限公司
