Release date:2020-05-11
Clinical & Experimental Allergy
[IF:5.158]
Maternal psychological distress before birth influences gut immunity in mid-infancyDOI: 10.1111/CEA.13551
Abstract:
Background: Maternal pre-postnatal psychosocial distress increases the risk for childhood allergic disease. This may occur through a host immunity pathway that involves intestinal secretory Immuno-globulin A(sIgA). Experimental animal models show changes in the gut microbiome and immunity of offspring when exposed to direct or prenatal maternal stress, but little is known in humans.
Methods: 1043 term infants from the Canadian Healthy Infant Longitudinal Development (CHILD) birth cohort were studied. Trajectories of maternal perceived stress and depression were based on scored-scales administered in pregnancy and postpartum. sIgA was quantified in infant stool (mean age 3.7 months) with Immundiagnostik ELISA. Linear and logistic regression were employed to test associations.
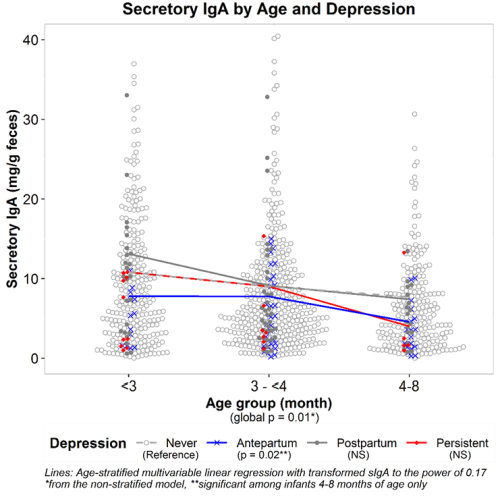
Results: Very low fecal sIgA concentrations were more common in infants of mothers in the antepartum and persistent depression trajectories (6% and 2% of women respectively). Independent of breastfeeding status at fecal sampling, infant antibiotic exposure or other covariates, the antepartum depressive symptom trajectory was associated with reduced mean infant sIgA concentrations (β= -0.07, p<0.01) and a 2-fold risk for lowest quartile concentrations (OR, 1.86; 95% CI: 1.02, 3.40). This lowering of sIgA yielded a large effect size in older infants (4-8 months) – breastfed and not. No associations were seen with postpartum depressive symptoms (7% of women) or with any of the perceived stress trajectories.
Conclusions: Despite improved mood postpartum and independent of breastfeeding status, mothers experiencing antepartum depressive symptoms delivered offspring who exhibited lower fecal sIgA concentrations especially in later infancy. The implications of lowered sIgA concentrations in infant stool are altered microbe-sIgA interactions, greater risk for C. difficile colonization and atopic disease in later years.
2020-02-17 Article
 杭州浙大迪迅生物基因工程有限公司
杭州浙大迪迅生物基因工程有限公司
